In the world of dental treatments, there are numerous options to enhance your smile, even if you have missing teeth. Understanding the possibilities and limitations of these treatments is crucial. This blog delves into whether veneers are a viable option for those with missing teeth and explores alternative treatments.
How to Treat a Missing Tooth
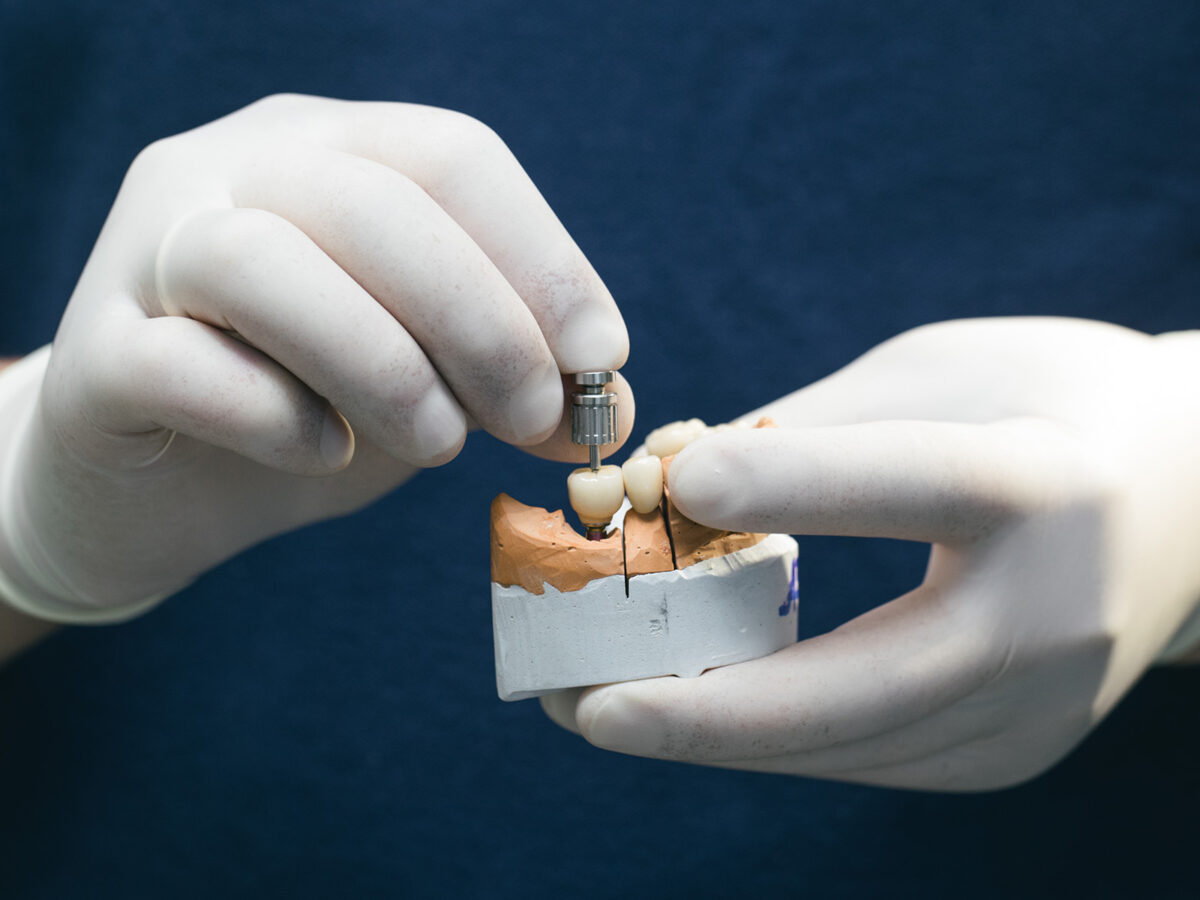
Modern dental technology offers several reliable and effective methods for replacing missing teeth. Among these, dental implants stand out as a popular choice. These metal posts act as artificial roots for replacement teeth and offer a permanent solution unlike dentures and bridges, which may require frequent adjustments and can become loose over time.
The Veneer Placement Process With Missing Teeth
Getting veneers typically involves three visits to the dentist. The process includes:
- Initial Consultation: The dentist evaluates your oral health and discusses your aesthetic goals. This step is crucial for addressing any concerns and planning the treatment.
- Preparation: A small amount of enamel is removed from the front surface of your existing teeth to ensure the veneers fit properly and stay in place.
- Design and Manufacture: If you have missing teeth, veneers are custom-designed to create a cohesive and natural-looking smile.
- Bonding: Once ready, the veneers are bonded to your teeth using dental adhesive. Adjustments are made to ensure optimal fit and appearance.
Alternatives For Missing Teeth
If you have missing teeth, consider these alternatives to veneers:
- Dental Crowns: These are ideal for replacing a single missing tooth, enhancing both aesthetics and functionality. Crowns fit over a damaged or decayed tooth, restoring its appearance and strength.
- Dental Implants and Bridges: These offer effective solutions for missing teeth. Implants provide a permanent replacement, while bridges are attached to neighboring teeth or implants.
- Orthodontic Treatments: In some cases, a combination of veneers and orthodontic treatments may be necessary to correct misalignments, improving overall smile aesthetics.
Conclusion
If you have missing teeth, it’s important to weigh your restoration options. While veneers can enhance your smile by covering gaps, misalignments, and stains, dental implants might be a better choice for missing teeth. Implants address not only aesthetic concerns but also prevent bone loss and other oral health issues. Veneers, on the other hand, are thin shells bonded to the front of natural teeth, primarily addressing cosmetic issues.
In summary, while veneers can improve the appearance of your smile, they are not a solution for missing teeth. For such cases, dental implants offer a more comprehensive and long-term solution. Always consult with a dental professional to determine the best course of action for your specific needs.